Stress Fractures and Bone Stress Injuries in Runners: What You Need to Know
As a runner, there’s nothing worse than being sidelined by an injury—especially one that sneaks up on you. Bone Stress Injuries (BSIs), often referred to as stress fractures, are among the most dreaded injuries for runners. You're not alone in this; they are a common experience for many runners.
They develop over weeks or months, making them difficult to diagnose early on. Sometimes, they take months to show up on X-rays or other tests.
But armed with a bit of knowledge, you can absolutely prevent and manage them well.
Whether you’re training for Around the Bay in Hamilton, the TCS Toronto Waterfront Marathon, another race, or simply enjoying regular runs, understanding BSIs is a powerful tool for staying injury-free.
Here's a run-down of the basics of BSIs, including updates from a recently published Expert Consensus in the Brutish Journal of Sports Medicine.
Is it a Bone Stress Injury or a Stress Fracture?
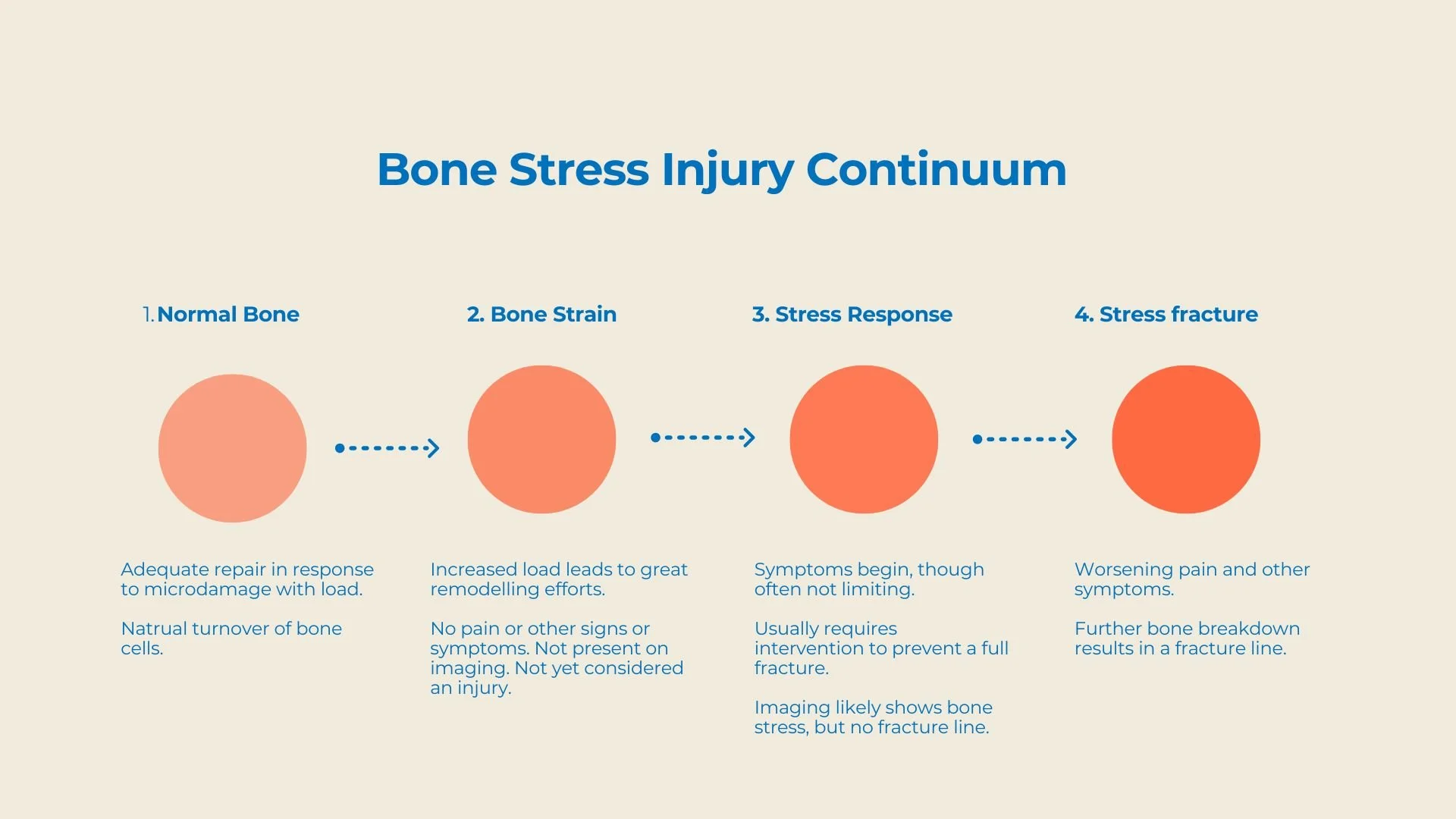
Bone Stress Injury (BSI) is the current term for what used to be called stress fractures, fatigue fractures, or bone marrow lesions. While these older terms are still used, it's important to note that BSI is a broader term that encompasses a range of injuries that occur when bones are repeatedly stressed. A stress fracture specifically refers to a small crack in the bone due to repetitive stress.
Several classification systems exist for BSIs, but there’s a promising movement toward adopting a single, universally accepted system. This could improve the accuracy of diagnosing and treating BSIs, giving runners hope for better injury management.
How Do Bone Stress Injuries Happen?
BSIs occur when a bone is repeatedly stressed beyond its ability to repair itself. Think of it like a continuum: the bone experiences microdamage but doesn’t have enough time to heal before the subsequent stress comes along. Over time, this damage can accumulate, and if not addressed, it can lead to a complete fracture.
Here’s a typical progression of how BSIs develop:
Increased Bone Remodeling is not yet considered an injury or a cause of pain; this is the stage where increased load leads to increased repair and cell turnover activity within the bone.
Initial stress-related damage: Microdamage occurs at a rate faster than the bone can repair itself.
Repeated microdamage: Continued stress causes more tiny cracks.
Bone fracture: The damage builds up to a point where a complete fracture occurs.
In the early stages, imaging like X-rays may not show any signs of injury, making diagnosing BSIs difficult. However, the damage still happens, and if not managed properly, the injury can worsen, potentially leading to a complete fracture and a more extended recovery period. This underlines the importance of early detection and proper management of BSIs.
Common Sites for BSIs in Runners
BSIs can happen in various parts of the body, but some areas are more vulnerable than others in runners:
Feet: The metatarsals and navicular are common trouble spots. Navicular stress fractures, particularly those in the fifth metatarsal, are particularly concerning because they have poor blood supply and are slow to heal. These injuries require more time off from running to ensure proper healing.
Shins: The tibia (shin bone) is a common site for BSIs. The good news is that tibial
stress fractures are usually quick to heal and are considered low-risk injuries. Less commonly, the fibula may also be affected.
Hips and Pelvis: Femoral neck and sacral BSIs are more serious because they heal slowly. For effective recovery, these injuries may require a period of non-weight-bearing activity.
How Are Bone Stress Injuries Diagnosed?
If you suspect a BSI, a physiotherapist, chiropractor, or doctor will likely begin by asking about your recent training.
Have you increased your mileage or intensity? They’ll also assess your risk factors, such as low vitamin D or low energy availability, which can contribute to bone weakness.
Key diagnostic methods include:
Patient History: A detailed discussion about changes in your training routine.
Physical Examination and Functional Tests: Specific tests (like the vertical single-leg hop test) can help pinpoint the injury and rule out other possible diagnoses.
Imaging:
X-rays are often the first step, but they may miss stress injuries.
MRI is considered the gold standard for diagnosing BSIs, offering a detailed view of the bone. However, there can be a long wait time for an MRI. If a BSI is suspected, it is often treated as one, even without imaging.
Other Imaging: In some cases, ultrasound or CT scans may be used, though these are less common.
The most recent expert consensus statement notes that although imaging helps, overdiagnosis is a concern. Therefore, it's crucial to consider imaging as part of the overall diagnostic picture.
What Are the Risk Factors for Bone Stress Injuries?
There’s no single cause of BSIs. Several factors can contribute to your risk, including:
Training Factors: Sudden increases in training volume or intensity are among the most common causes of BSIs. Gradually ramping up your training can help prevent this.
Bone Health: Low bone density, poor nutrition, and Relative Energy Deficiency in Sport (RED-S) can weaken bones. A nutritionist or dietitian can help ensure your diet supports strong bones.
Biomechanics: Poor running form or incorrect footwear can increase your risk of BSIs. A physiotherapist or chiropractor can assess your running mechanics to help reduce your risk.
Understanding Low Energy Availability and RED-S
Inadequate fuelling plays a key role in many BSIs, so it’s essential to understand if this may apply to you.
Relative Energy Deficiency in Sport (RED-S) is the term for the interrelated and multisystemic health and performance outcomes that occur when an athlete doesn’t consume enough calories to support both their physical activity and daily life.
Among many other multi-systemic concerns, this can lead to bone health issues, including BSIs. Women and those who menstruate, athletes with low body mass, those with irregular menstrual cycles, and those who don’t get enough calories are particularly at risk. It’s crucial to address RED-S with a comprehensive approach, including a sports physician for medical management, a dietitian for nutritional guidance, and a physiotherapist for exercise and rehabilitation planning.
Common Signs and Symptoms of Bone Stress Injuries
Here are some signs to watch for if you suspect a BSI:
Weight-bearing pain: Pain with walking, hopping, or running.
Pain behaviour: Unlike other injuries, BSIs don’t improve with warming up and may worsen as activity continues.
Tenderness: Pain is usually localized to a specific area of the bone, such as the front of the tibia. It’s usually a fairly concentrated area (no more than a finger width or two) rather than the length of the bone or a significant portion thereof.
Swelling: You might notice swelling in more superficial bones like the tibia, though deeper bones like the femoral neck may not show this.
Previous Injuries: If you've had a BSI before, you’re at higher risk of another one.
How Are Bone Stress Injuries Treated?
The good news is that most BSIs can be treated with conservative care:
Rest: Especially when we consider that BSIs occur due to the load on your bones exceeding their capacity for repair, reducing that load is key to recovery.
Gradual Return to Running: Once healed, you’ll need a structured, gradual plan to ease back into running.
Professional Help: If the injury is severe or you have a high-risk BSI, consulting a physiotherapist, chiropractor, or doctor is essential to ensure a safe recovery.
Innovative Treatments for Bone Stress Injuries
While rest and gradual return-to-sport plans are the mainstay of treatment, new options are emerging:
Shockwave Therapy: This treatment strategy uses sound waves to stimulate your body’s cascade of healing strategies in the damaged bone tissue.
Antigravity Treadmills: These specialized treadmills allow you to run on a reduced percentage of your body weight, decreasing loads on your bones and allowing you to maintain fitness while minimizing stress on your body.
Footwear Technology: Advances in running shoe technology may help reduce bone stress, though more research is needed.
These treatments show promise, but you should discuss them with a qualified professional to determine if they’re appropriate for your specific injury.
Returning to Sport After a BSI
When you’re ready to return to running, it’s essential to do so carefully. A step-by-step plan ensures that the injury heals fully and you can successfully return to pain-free running and training. Working with a physiotherapist, coach, or sports medicine doctor is a good idea to develop a safe, gradual return-to-sport strategy.
Conclusion: Preventing and Recovering from Bone Stress Injuries
Bone stress injuries can seriously damper your running routine, but you can prevent them by understanding how they develop and taking proactive steps. Gradual training increases, proper nutrition, and attention to running mechanics are key to keeping your bones strong and healthy.
At our run-focused clinics in Toronto and Hamilton, our team includes physiotherapists, chiropractors, and other clinicians who specialize in helping runners avoid and recover from BSIs. If you're experiencing pain or discomfort, contact us for an assessment and personalized treatment plan through the lens of your running goals. With the proper care, you'll be back to your regular running routine—injury-free—in no time, which also means finding more joy in the process!